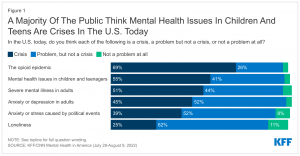
Join the Children & Youth Behavioral Health Work Group’s efforts to improve mental health and substance use/alcohol treatment services and supports for children, young people through age 25, and their families.
There are several opportunities for you to participate:
- The Children & Youth Behavioral Health Work Group (CYBHWG)
- The Prenatal-25 Behavioral Health Strategic Plan Advisory Group (P-25 Strategic Plan Advisory Group)
- The P-25 Strategic Plan Advisory Group parent/caregiver and youth/young adult subcommittees
These opportunities are described more fully below.
- To become a member of the Children & Youth Behavioral Health Work Group (CYBHWG) or the P-25 Strategic Plan Advisory Group, you must nominate yourself/apply. Information about how to nominate and/or apply is included below (attached form for CYBHWG and survey links for P-25 Strategic Plan Advisory Group).
- The P-25 Strategic Plan Advisory Group parent/caregiver and youth/young adult subcommittees are open to all and information to sign up to join these meetings is also included below.
Please note the following supports that are available:
- Most parent/caregiver and youth/young adult members of the CYBHWG and the SPAG may receive payment for attending meetings.
- All parent/caregiver and youth/young adult attendees at the strategic plan subcommittee meetings described below who meet the above criteria may receive payment for attending meetings.
- Child and elder care, as well as travel expenses for in-person meetings, are also covered.
- Translation and interpreter services are available, if arranged in advance.
We can’t improve the system without you – your experience and wisdom will ensure that these services truly look and feel like help to those who seek them.
If you have questions or need more information, please send an email to cybhwg@hca.wa.gov.
1. Children & Youth Behavioral Health Work Group (CYBHWG)
The CYBHWG currently has openings for one parent or caregiver and two young people between the ages of 13 and 29 who have had experience with mental health or drug and alcohol-related programs or services.
The CYBHWG is a group of legislators, state agency representatives, health care providers, tribal governments, community behavioral health services, advocates, young people who have received behavioral health services (mental health and/or substance use/alcohol treatment), and parents of children and young people who have received services. Each year this group provides recommendations to the Governor and the Legislature to improve behavioral health services and strategies for children, youth, young adults, and their families – and each year many of these recommendations are passed into law.
Additional Details
Time commitment: Attend up to eight 3-4 hour CYBHWG meetings per year and one 3-hour member retreat. Most meetings are virtual (held on Zoom). All in-person meetings include a virtual option.
Term: Member terms may not exceed 3 years.
Application deadline: Wednesday, May 8, 2024
To nominate yourself: Please use the attached 2024 CYBHWG nomination form.
To nominate someone else: Please send their name and why you think they should be on the CYBHWG to amber.leaders@gov.wa.gov and cybhwg@hca.wa.gov, and cc the person you’re nominating.
CYBHWG meetings are open public meetings. Each meeting includes a public comment period; some also include breakout groups in which non-members can participate.
2. Prenatal-25 Behavioral Health Strategic Plan Advisory Group
The CYBHWG is currently developing a statewide strategic plan to improve the behavioral health system for all of Washington’s children, youth, young adults, and their families.
The goals for the Prenatal-25 Strategic Plan:
- Develop a long-term system-wide strategy and roadmap to build robust, equitable services and supports from prevention through intensive inpatient services.
- Engage deeply with communities and stakeholders and sustain an ongoing feedback loop.
- Drive tangible improvements along the way.
Its guiding principles include:
- No wrong door.
- Help that looks like help.
- Informed by children, youth and families that utilize services
- Oriented toward prevention to avoid future crises and reduce the need for more intensive services
The P-25 Strategic Plan Advisory Group is made up of parents, young people, and system partners. The advisory group will serve as a platform to bring all partners together to find common ground and develop collective suggestions.
Additional Details
Time commitment: Up to five 3-4 hour meetings per year and one 3-hour member retreat, plus review of draft documents and other materials as needed.
Most meetings are virtual (held on Zoom). All in-person meetings include a virtual option.
Term: Member terms may not exceed 2 years.
Application deadline: extended to Wednesday, May 8, 2024
To apply for membership on the P-25 Strategic Plan Advisory Group, please use the links below:
To nominate someone else: Please send their name and why you think they should be on the CYBHWG to amber.leaders@gov.wa.gov and cybhwg@hca.wa.gov, and cc the person you’re nominating.
3.The Prenatal-25 Spag Parent/Caregiver And Youth/Young Adult Subcommittees
Come to our monthly Parent/Caregiver and Youth/Young Adult subcommittees!
Throughout the year, we will be holding monthly 1-2 hour meetings to share progress and plans and get your ideas and input. Every meeting is open to any parent or young person who wants to attend; there are no appointed members. We will begin scheduling these meetings in May. If you are interested in participating in one of these subcommittees, please send email to cybhwg@hca.wa.gov and we’ll add you to the mailing list.
Additional Details
Time commitment: Attend monthly 1-2 hour meetings, as you are available.
We welcome your participation, even if you can only attend occasionally.
Presentation To Your Group or Organization
We are happy to come to your group’s meetings or gatherings – in person or virtually – to share information about the Prenatal-25 Strategic Plan and get your ideas for how to create a better system. Please email cybhwg@hca.wa.gov if you know of groups or people we should connect with.
We are grateful for the opportunity to work in partnership with young people, parents, and community members.